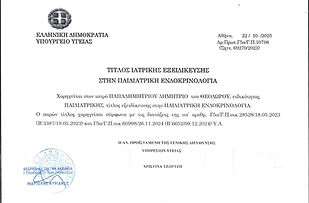
Dr. Dimitris T. Papadimitriou
Pediatric Endocrinologist - Pediatric Diabetologist DIU, DU, CCU,
former Lecturer at Joseph-Fourier University, Grenoble, France
Visiting Professor of Neonatal - Peditaric - Adolescent Endocrinology at the University of Thessaly Medical School, as of the academic year 2023-2024
Parents affronting adolescent disorders
The improvement of the diet, but also the abundance of food - but mainly of the "garbage food" - together with the improvement of the general health of the children and their faster psychosocial maturation, possibly with the contribution of other factors (eg plant- estrogens in food), have led to a persistent trend of advanced age-related secondary sex characteristics. At the same time, the improvement of the socio-economic level but also the development of the subspecialties of pediatrics brings the parent more often faced with puberty disorders (eg constitutive growth retardation and adulthood, advanced puberty).
Awareness is the transition from childhood to adulthood. It is characterized by hormonal, morphological and psychological changes. A pathological puberty (late, premature or abnormal) will affect both the child and his family.
Puberty is characterized by sexual maturation manifested as:
- the growth of the gonads (testicles, ovaries)
- the development of secondary gender characteristics
the acceleration of height growth
This maturation starts with the "awakening" of an upper brain center, the hypothalamus, and the consequent stimulation of the hypothalamic-pituitary (endocrine gland) axis of the gonads, resulting in the secretion of sex steroids (estrogen) and estrogen. to fertility.
Various factors determine the age of onset of puberty: genetic, racial, nutritional and mental. Internationally, there is a tendency for puberty to begin at a younger age, especially in girls.
While the triggering mechanism for hypothalamus in the brain is not yet sufficiently elucidated, when this occurs, the gonadotropin-releasing factor (LHRH) is secreted by hypothalamic neurons, which also causes the coronary artery LH) from the pituitary gland, events that precede 1 to 2 years of the appearance of clinical signs of puberty. This phenomenon, which occurs mainly during nighttime sleep, is constantly increasing in frequency and intensity, leading to successive stimulation of the pituitary gland, gonads and eventually all target tissues of sex steroids. About one to two years ago, the adrenal glands already began to secrete hormones, which are primarily responsible for the development of pubic hair and armpits as well as the acceleration in the rate of growth that can be observed before the signs are even clinically perceived. of puberty.
The development of secondary sex characteristics is codified by pediatric endocrinologists based on Tanner's ranking from 1 to 5, with stage 1 corresponding to preadolescent appearance and stage 5 to full adult development.
The first sign of puberty in a girl, around the age of 10 (8-13), is the development of a palpable mammary gland (often unilateral in the beginning), accompanied (followed or followed) by the presence of hair in the adolescent. Armpit hair comes 1-1.5 years later. The interval between this initial stage and the menarche (period) is about 2 years. The period acquires its full cyclical character within about 18 months from its onset, as the first cycles are usually if they are non-ovulatory.
Ultrasound (uterine - ovarian ultrasound) and hormonal data (measurement of estradiol and gonadotrophs usually after a challenge examination lasting 60΄- 90΄) complete the clinics to assess adolescent maturity in the girl.
In the boy, the first sign of adolescence (which is not easily detected by parents) is the increase in testicular volume (average age 11.5 years). Dimensions> 25 x 15 mm (using a simple measuring tape) or volume> 3 ml (using an orchidometer) means activation of the hypothalamic-pituitary-testicular axis. Quite often (30%) this activation can follow after 1-2 years of mild gynecomastia, which in most cases is temporary. However, gynecomastia in boys always requires endocrinological examination to rule out mainly hormone-producing tumors. It is noted that in several cases it can be successfully treated with medication, while if it is installed for more than two years, the final solution can be given only by plastic surgery after the completion of puberty.
In both sexes, the growth rate accelerates in adolescence from the pre-adolescent rate of 5-6 cm / yr to 7-9 cm / yr. The difference is that girls show the maximum growth rate about 1 year after the onset of adolescence (11-12 years), while boys up to 2 years after adolescence (13-14 years). Also characteristic, especially in boys, is the slowdown in growth rate - which can reach the lower limit of normal, ie 4 cm / yr - the year preceding the maximum growth rate. On average, girls will grow 25 cm tall and boys 28 cm during puberty. Thus the final height of the child depends to a large extent on the height he had at the beginning of puberty.
Important time points (years)
Normal puberty 9-13 (boy) 10-14
Early puberty (girl) <8 (boy) <9
Advanced pub (girl) 8-9 (boy) 9-10
Late puberty (girl)> 13 (boy)> 14
Advanced development is called the development of secondary sex characteristics:
-
before 8 years in the girl: appearance of breasts and / or hair of a teenager
-
before 9 years in the boy (20 times rarer): increase in testicular volume> 3 ml (size> 25 x15 mm) and / or adolescent hair.
In the face of an early or advanced puberty one must distinguish whether it is a central (true) early puberty, characterized by the early activation of the neuroendocrine axis hypothalamus - pituitary - gonads and controlled by upper brain centers, or peripheral early puberty or pseudobulb, independent of the brain, due to masculinization or feminization due to autonomous production of sex hormones by the testicles, ovaries and adrenal glands.
Without inhibition of early puberty, the final height is usually significantly lower than the target height (calculated from the average height of the parents -6.5 cm for the girl and +6.5 cm for the boy), due to the advanced bone maturation. Another equally important parameter is the manifestation of adolescent behavior with possible consequences on sexual maturity and school performance and of course the most complete fertility at a very young age.
Special care is needed in cases of advanced and sometimes early puberty that correspond to a peculiar acceleration of growth and onset. This is usually accompanied by a relatively tall stature for age, as well as advanced bone age, which, however, moves exactly on the curve of the theoretical height - target. In most cases, the same thing has happened to one of the parents, who is of normal height. Studies have shown that terminating puberty in these cases has no benefit, at least in terms of final height. The distinction is subtle and follow-up is required to confirm this diagnosis. Recognition of this physiological variant is important to avoid over-treatment with pubertal inhibition regimens.
So the first thing we need to document is whether the onset of puberty is early or advanced. If it is early, there should be a clinical and etiological investigation to rule out any pathology, while if it is advanced, a simple follow-up may suffice. The centers that control the onset of puberty are located in the brain. Therefore, in rare cases, a tumor or cyst may have activated "early puberty". In contrast, tumors of the ovaries, testes, or adrenal glands can produce estrogen or androgens on their own, and we have a clinical picture of puberty due to peripheral causes (not of the brain).
The family environment on the other hand plays a catalytic role in activating the mechanisms of puberty. The more love, nourishment and care there is, the faster the maturation process of the child will begin. A typical example is the children of the 3rd world who are adopted in European countries. They show early puberty at the ages of 5, 6, or 7 years, which shows that these children, deviated from love, food and care, are suddenly found in families where there is an oversupply of those who were deprived and therefore show puberty.
Let us now look at some medical conditions that parents can deal with
Early Breastfeeding
is called the isolated occurrence of unilateral or bilateral non-painful mammary gland in girls <7 years, with the most frequent occurrence at the age of 6 months - 3 years. It is known that at the age of 6-18 months there is a normal activation of the pubic axis in females (femaleminipuberty), an overactivity of which can lead to early breastfeeding. There are no other signs of feminization, no significant acceleration of growth, nor very advanced bone maturation. Breast growth is transient and can progress for 6-18 months. Care should be taken in monitoring these girls as an early mammal may be the first sign or develop into a central early puberty, especially around the age of 5 years.
Early adrenaline
is called the early isolated appearance of hair in the adolescent and / or armpit, before the age of 8 years in both boys and girls. Probably due to early activation of the adrenal glands but also to increased sensitivity to androgens of target tissues. Bone age may be a little advanced. Adrenal androgens are elevated with age but are compatible with the Tanner stage of puberty. Hormonal examination will allow the exclusion of a disease or tumor of the adrenal glands.
In addition to early or advanced puberty, parents are often faced with late adolescence.
Delayed puberty
we have when there is no breast development in the girl at the age of 13 years and we do not have an increase in testicular volume in the boy (<4 ml or <25 x 15 mm) at the age of 14 years.
Clinical orientation is based on family history: puberty (maternal age 1, paternal adolescence), anosmia-hyposmia (Kallmann syndrome), cryptorchidism (bilateral), infertility in family members (possible hypogonadism) and souvenir with the curve of height and weight and speed of increase, body mass index (eating disorders, malabsorption, celiac disease).
Constituent delay of puberty is diagnosed as exclusion after pathological causes are ruled out: adolescent development eventually occurs normally, but with a long time delay. After the complete investigation and clarification of the etiology of delayed puberty, we proceed to both the treatment of the cause and the treatment of hormone replacement if necessary. In other words, we can use small doses of androgens or estrogens to "wake up" puberty when it is very late and thus creates psychological problems in children, both because they are less physically mature than their peers, and because along with maturation is delayed. height increase, often creating a feeling of inferiority.
Primary amenorrhea
is called the non-arrival of the period at the age of 16 years (menstruation follows about 2 years after the onset of puberty). It can be due to serious endocrine causes and needs urgent control, especially when combined with short stature.
Of course, endocrine control always requires Secondary amenorrhea (interruption of an already established normal cycle), which can hide serious endocrine problems in addition to the most common and perhaps the most common problem of polycystic ovaries.
Treatment
As far as the treatment of early puberty is concerned, we are essentially fooling the system that activates central adolescence. It is done in a way that does not involve risks or side effects. With a subcutaneous injection at another time interval (from 1 to 3 months depending on the case) we give the child a hormone that is produced by the body itself (LHRH) and is involved in the onset and development of puberty. It is a painless method (subcutaneous formulations) for the child, but it should not be started before it is clarified whether it is an early or advanced puberty and whether the child is really going to benefit from this treatment either in terms of height or in terms of psychological and psycho-social.
In conclusion, we must point out a common omission of parents, is that as soon as the vaccinations end, the visits to the pediatrician stop, unless the child becomes ill. As long as there is not even one annual visit, it is impossible to assess whether the child's physical and mental development is developing normally. So many times the parents turn to the pediatric endocrinologist when the "early puberty" is at an advanced stage, which makes the treatment even more difficult and its results definitely poorer. So let's get the message across to all children, at least once a year to visit their pediatrician. Greek parents must understand that the pediatrician is not just for diseases. After all, prevention is the best treatment.
And so that we do not focus only on the physical changes, let us not forget that the child changes behavior from the very early stages of adolescence. It usually becomes more reactive, more absolute and very demanding, while it often closes in on itself.

